Discover the real daily lifestyle of working nurses—from 12-hour shifts to work-life balance challenges. A registered nurse shares authentic insights into nursing routines, burnout, and health strategies.

Introduction
It’s 6:45 AM, and your alarm pierces through the darkness. You have exactly 45 minutes to shower, fuel your body, pack your meals, and drive to the hospital for a 12-hour shift that will likely stretch to 13 or 14 hours. This isn’t just one day—it’s the reality for millions of nurses across America, repeated three to five times every week.
As Abdul-Muumin Wedraogo, a Registered General Nurse with over 10 years of clinical experience across Emergency, Pediatric, Intensive Care, and General Ward settings, I’ve lived this reality firsthand. The romanticized image of nursing—compassionate care, grateful patients, and fulfilling work—tells only part of the story. The complete picture includes physical exhaustion, emotional strain, missed family dinners, and the constant juggling act between providing excellent patient care and maintaining your own well-being.
Nearly 5.2 million registered nurses work nationwide National University, making nursing America’s largest healthcare profession. Yet behind these statistics are real people navigating one of the most demanding careers imaginable. Over 138,000 nurses departed from the workforce between 2022 and 2024 Advisory, with burnout, stress, and workload pressures cited as primary reasons.
This article provides an unfiltered examination of what nurses’ daily lives actually look like—from the moment we wake up until we collapse into bed, and everything in between. Whether you’re considering nursing as a career, supporting a nurse in your life, or simply curious about what happens behind hospital doors, this comprehensive guide reveals the authentic experience of modern nursing.
Disclosure: This article contains affiliate links. As an Amazon Associate and affiliate partner of various medical device retailers, Muminmed.com earns from qualifying purchases. This comes at no additional cost to you and helps support our work in providing evidence-based health information. All recommendations are based on clinical experience and research.
Table of Contents
The Reality of Nursing Schedules: More Than Just “Three Days a Week.”
The 12-Hour Shift Standard
“You only work three days a week? That must be nice!” If you’re a nurse, you’ve heard this countless times from well-meaning friends and family. The reality is far more complex.
Working 12-hour shifts has become standard for many hospital nurses, typically from 7 AM to 7 PM or 7 PM to 7 AM, American Nurses Association. These extended hours mean nurses provide 24-hour continuous patient care with fewer handoffs between shifts, theoretically improving care continuity.
The Math Doesn’t Add Up
Let’s break down what “three days a week” actually means:
- Work hours: 12 hours (often extending to 13-14 hours)
- Preparation time: 1-2 hours (showering, dressing, packing meals, commuting)
- Recovery time: 3-4 hours (decompressing, eating, showering after shift)
- Sleep needed: 8-10 hours (often only getting 5-7 hours)
Total time consumed per work day: Approximately 24-28 hours when you factor in recovery
Each work shift essentially equals two days when considering preparation and recovery, Nurse.org. Night shift nurses must sleep before working and again after their shift, meaning a single work night can consume two full days.
Common Scheduling Patterns
Three-Day Consecutive Schedule
- Work Monday, Tuesday, Wednesday
- Off Thursday through Sunday
- Advantage: Four consecutive days off
- Disadvantage: Severe cumulative fatigue by day three
Spread-Out Schedule
- Work Monday, Tuesday, off Wednesday, Thursday, work Friday
- Advantage: Recovery time between shifts
- Disadvantage: Never truly “off” for extended periods
Four-Day 10-Hour Shifts. In outpatient settings, nurses often work four 10-hour shifts weekly, Nursejournal.org, offering slightly more manageable days while still providing three days off.
The Hidden Hours
Nurses must complete handoff reports to incoming staff, and necessary patient care often extends beyond the scheduled 12 hours. Arriving 15 minutes early to review patient charts and staying 30-60 minutes late to complete documentation is common, although it is often unpaid.
From my experience in the ICU, leaving “on time” was rare. Critical patients don’t conveniently stabilize at 7 PM, and abandoning care mid-crisis isn’t an option. These extra hours add up—sometimes an additional 5-10 hours per week.
Weekend and Holiday Work
Nurses must work weekends to ensure 24/7 coverage, which creates challenges for those with families or weekend commitments. Christmas, Thanksgiving, New Year’s—healthcare doesn’t pause for holidays. Most nurses rotate holiday coverage, meaning you’ll work major holidays regularly throughout your career.
A Typical 12-Hour Shift: Hour-by-Hour Breakdown
Morning Preparation (5:30 AM – 7:00 AM for Day Shift)
5:30 AM: Alarm goes off. Hit snooze once (maximum), then force yourself up.
5:45 AM: Quick shower, throw on scrubs, minimal makeup or grooming. Efficiency is key.
6:00 AM: Breakfast—often something quick like oatmeal, a protein shake, or scrambled eggs. Pack lunch, snacks, and water bottles (2-3 liters minimum).
6:30 AM: Commute. Use this time for mental preparation or catch up on audiobooks/podcasts to decompress.
Beginning of Shift (7:00 AM – 9:00 AM)
7:00 AM: Arrive 15 minutes early (unpaid) to review patient charts and gather supplies before receiving the handoff report.
7:15 AM: Handoff report from night shift. Receive critical patient information—diagnoses, vital signs, medications, procedures, and family concerns. Take detailed notes.
7:45 AM: Begin initial patient assessments. Check vital signs, perform head-to-toe assessments, review overnight labs and diagnostic results.
From my emergency nursing experience, these first two hours set the tone for your entire shift. A calm morning can quickly spiral into chaos with new admissions, deteriorating patients, or emergencies.
Mid-Morning Rush (9:00 AM – 12:00 PM)
9:00 AM: Medication administration begins—the “med pass.” Depending on your patient load, this can take 1-2 hours.
10:00 AM: Procedures, treatments, and care activities. Wound care, catheter insertions, IV starts, blood draws, and assistance with activities of daily living.
11:00 AM: Documentation catch-up. Chart everything you’ve done so far—assessments, medications, treatments, patient responses.
11:30 AM: Brief bathroom break if you’re lucky. Many nurses go 4-6 hours without urinating due to overwhelming patient demands.
Midday Challenges (12:00 PM – 3:00 PM)
12:00 PM: Attempt to eat lunch. Often interrupted for emergencies, admissions, or patient call lights. Many nurses eat standing up or skip meals entirely.
12:30 PM: New admissions or discharges. Process paperwork, conduct admission assessments, and educate patients and families.
1:00 PM: Second round of assessments and medications. Some medications require administration every 4-6 hours.
2:00 PM: Continued patient care, answering call lights, assisting with mobility, changing linens, and repositioning patients to prevent pressure ulcers.
Patient ratios for 2023 showed 76.3% of CNAs, 92.3% of LPNs, and 62.9% of RNs regularly cared for 9 or more patients during a typical shift. These numbers directly impact how much time you can dedicate to each patient.
Afternoon Grind (3:00 PM – 6:00 PM)
3:00 PM: Another medication round. By now, fatigue is setting in, but vigilance cannot waver—medication errors are most common during peak fatigue periods.
4:00 PM: Family phone calls and visitor management. Explain treatment plans, address concerns, and coordinate with physicians.
5:00 PM: Final assessments before shift change. Gather all information needed for a comprehensive handoff.
6:00 PM: Catch up on documentation. Everything must be charted before handoff—and that’s often 30-60 minutes of focused typing.
End of Shift (6:30 PM – 7:30 PM)
6:45 PM: Prepare handoff report for incoming night shift. Organize thoughts, prioritize critical information.
7:00 PM: Give report to night shift nurse. Typically 15-30 minutes per patient, depending on complexity.
7:15 PM: Final check of patients, ensure nothing critical is pending, gather personal belongings.
7:30 PM: Clock out (hopefully). Exhausted commute home.
Post-Shift Reality (8:00 PM – 10:00 PM)
8:00 PM: Arrive home physically and emotionally drained. Shower immediately—hospital germs don’t belong in your home.
8:30 PM: Eat dinner, often reheating leftovers or takeout. Too tired to cook.
9:00 PM: Attempt quality time with family, but your mental capacity is diminished.
9:30 PM: Prep for next shift if working consecutively—pack meals, set out scrubs.
10:00 PM: Bed. You need 8 hours of sleep, but will probably get 6-7 before repeating tomorrow.
[Table: Typical 12-Hour Day Shift Breakdown]
| Time | Activity | Notes |
| 7:00-7:45 AM | Handoff & Report | Unpaid arrival time is often 6:45 AM |
| 7:45-9:00 AM | Initial Assessments | All patients must be assessed |
| 9:00-12:00 PM | Medications & Procedures | High-concentration required |
| 12:00-1:00 PM | Lunch (if possible) | Often interrupted or skipped |
| 1:00-6:00 PM | Continued Care & Documentation | Physical and mental fatigue increases |
| 6:00-7:00 PM | Final Documentation | Cannot leave until complete |
| 7:00-7:30 PM | Handoff Report | Unpaid overtime common |
The Physical Demands: Why Nursing is Like Athletic Training
Constant Movement and Physical Labor
Nurses spend significant time walking, bending, stretching, and standing, making them vulnerable to back injuries from frequently lifting and moving patients, according to the U.S. Bureau of Labor Statistics.
During a typical 12-hour shift, nurses:
- Walk 4-5 miles (approximately 10,000-12,000 steps)
- Lift or reposition patients weighing 100-300 pounds multiple times
- Stand for 8-10 of the 12 hours
- Perform repetitive motions (medication preparation, documentation, IV starts)
- Maintain awkward postures during procedures.
From my pediatric nursing experience, even working with smaller patients requires considerable physical effort. Holding struggling toddlers for procedures, running between rooms during emergencies, and constantly bending to child-height beds takes its toll.
Common Physical Health Issues
Musculoskeletal Problems
- Lower back pain (affecting 60-80% of nurses at some point)
- Knee and foot problems from prolonged standing
- Shoulder and neck strain from lifting
- Carpal tunnel syndrome from repetitive documentation
Varicose Veins and Circulatory Issues. Standing for extended periods causes blood pooling in the legs, leading to varicose veins, leg cramps, and an increased risk of blood clots.
Compression Stocking Reality: Many nurses wear compression stockings daily—not a fashion statement, but a medical necessity to prevent venous insufficiency.
Sleep Deprivation Effects
Night shift nurses face particular challenges. A 2021 study found nurses working night shifts experienced lower activity levels, poorer sleep quality, and reduced life satisfaction compared to day shift workers. Healthynursehealthynation.
Sleep deprivation causes:
- Decreased cognitive function and reaction time
- Increased risk of medication errors
- Weakened immune system
- Weight gain and metabolic dysfunction
- Mood disturbances and irritability
Infection Exposure
Nurses frequently encounter people with infectious diseases and regularly contact potentially harmful or hazardous drugs and substances, according to the U.S. Bureau of Labor Statistics. During my ER experience, exposure to bodily fluids, infectious diseases (including TB, COVID-19, influenza, and MRSA), and hazardous chemicals was a daily occurrence.
Personal protective equipment helps, but isn’t foolproof. Many nurses catch illnesses from patients, yet must continue working (often while sick) due to staffing shortages.
The Toll on Your Body
Think of nursing as a marathon you run three times a week, except you’re also solving complex problems, making life-or-death decisions, and emotionally supporting people through their worst moments—all while physically exhausted.
Your body needs recovery time equivalent to an athlete’s training schedule, yet nurses often return for consecutive shifts without adequate rest.
Nutrition and Meal Planning for Shift Workers
The Challenge of Eating Well
Maintaining proper nutrition as a nurse presents unique challenges:
- Unpredictable break times
- Limited access to healthy food options
- Vending machine temptations
- Exhaustion leading to poor food choices
- Disrupted circadian rhythms affect digestion
Night shifts disrupt circadian rhythms that regulate digestion and metabolism, according to Nurse.com, increasing risks for weight gain, insulin resistance, and gastrointestinal discomfort.
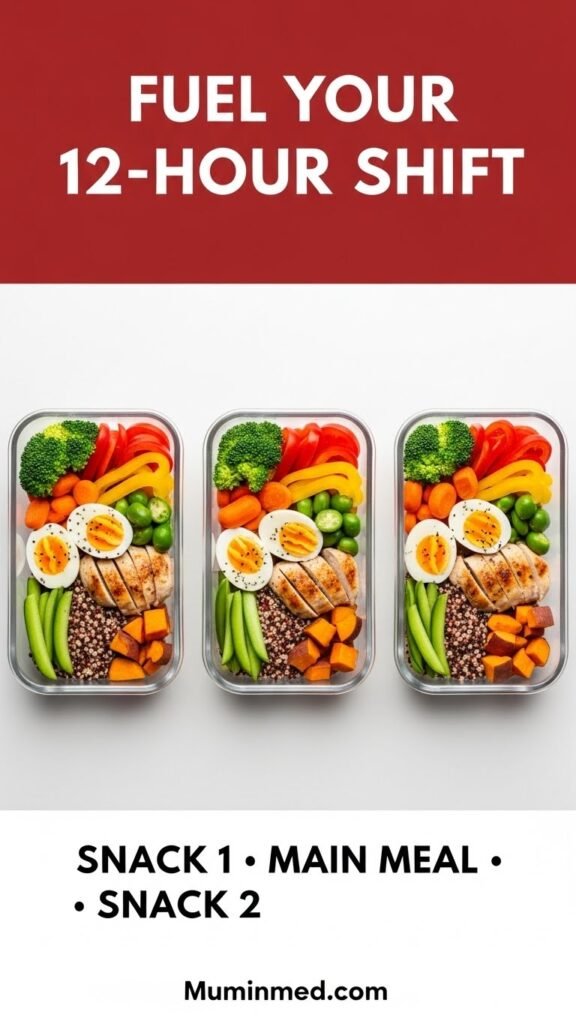
The Meal Prep Solution
Planning at least one meal and two snacks for a 12-hour shift is essential for NCLEX Practice Tests. Recommended timing:
- Snack 1: Several hours after shift start
- Main meal: Halfway through shift (around hour 6)
- Snack 2: Two hours before shift ends
What to Pack: Nutrient-Dense Choices
Proteins (Muscle Repair and Sustained Energy)
- Grilled chicken breast
- Hard-boiled eggs
- Greek yogurt
- Tuna or salmon pouches
- Lean turkey
- Lentils and beans
Complex Carbohydrates (Long-Lasting Energy)
- Quinoa
- Brown rice
- Sweet potatoes
- Whole-grain bread
- Oatmeal
Healthy Fats (Brain Function)
- Avocados
- Nuts and seeds
- Olive oil
- Salmon
Vegetables and Fruits (Vitamins, Minerals, Fiber)
- Pre-cut vegetables with hummus
- Baby carrots
- Cucumber slices
- Berries
- Apples
- Cherry tomatoes
Sample Meal Prep for Three 12-Hour Shifts
Breakfast (Before Shift)
- Overnight oats with berries and almonds
- Veggie egg muffins
- Protein smoothie
Snack 1 (Hours 3-4 of Shift)
- Mixed nuts with dried fruit
- Protein bar
- String cheese with whole-grain crackers
Main Meal (Hour 6-7 of Shift)
- Grilled chicken with quinoa and roasted vegetables
- Turkey and avocado wrap with a side salad
- Sweet potato with black beans and salsa
- Mediterranean bowl with chicken, cucumber, tomatoes, feta, and tzatziki
Snack 2 (Hours 10-11 of Shift)
- Apple with almond butter
- Greek yogurt with granola
- Vegetable sticks with guacamole
Post-Shift Meal
- Light, easily digestible meal
- Avoid heavy foods that disrupt sleep
Hydration is Critical
Even mild dehydration causes fatigue, headaches, and brain fog. Aim for:
- 2-3 liters of water per 12-hour shift
- Water bottle always accessible
- Limit caffeine to the first 6 hours of the shift
- Avoid energy drinks with excessive caffeine and sugar
Caffeine Strategy
Research shows caffeine consumed at shift start and during the first 4-6 hours can improve alertness and concentration, but avoid caffeine during the last half of your shift to prevent sleep disruption.
From personal experience, I learned this the hard way—drinking coffee at hour 10 of a night shift meant lying awake for hours after getting home, defeating the purpose of improved alertness.
What to Avoid
- Sugar and simple carbohydrates: Cause energy crashes
- Fried and heavily processed foods: Cause sluggishness and digestive discomfort
- Large meals: Difficult to digest during physically demanding work
- Excessive caffeine: Causes jitteriness and sleep problems
Realistic Expectations
Perfect nutrition during every shift isn’t achievable. Some days, you’ll eat vending machine pretzels standing at the nurses’ station. That’s reality. The goal is to make healthy choices most of the time and have nutritious options readily available.
[Table: Nurse-Friendly Meal Prep Recipes]
| Recipe | Prep Time | Key Nutrients | Why It Works |
| Mediterranean Quinoa Bowl | 30 min | Protein, Complex Carbs, Healthy Fats | Easily reheated, balanced macros |
| Turkey & Black Bean Burrito Bowl | 25 min | Protein, Fiber, Complex Carbs | Portable, filling, stable energy |
| Chicken & Veggie Stir-Fry | 20 min | Protein, Vitamins, Minerals | Quick prep, versatile flavors |
| Stuffed Bell Peppers | 40 min | Protein, Fiber, Antioxidants | Make ahead, freeze well |
| Greek Yogurt Parfait | 5 min | Protein, Probiotics, Antioxidants | Quick snack, gut health |
Sleep Challenges and Circadian Rhythm Disruption
The Science of Shift Work and Sleep
Our bodies evolved to sleep at night and be active during the day. Night shift nursing fights millions of years of biological programming, and your body knows it.
Night shifts disrupt the body’s circadian rhythms, which regulate digestion, metabolism, and sleep-wake cycles, according to Nurse.com. This disruption affects nearly every physiological system.
Night Shift Sleep Reality
The Double-Sleep Phenomenon. Night shift nurses must sleep before working and again after their shift, according to Nurse.org, meaning:
- Sleep Monday daytime
- Work Monday night
- Sleep Tuesday daytime
- Essentially, two full days are consumed by one work shift
Quality vs. Quantity Even when you get 7-8 hours of daytime sleep, it’s not equivalent to nighttime sleep. Daylight, noise, phone notifications, and family activities all fragment sleep quality.
Common Sleep Problems for Nurses
Insomnia After physically demanding 12-hour shifts, you’re exhausted but wired. Adrenaline from emergencies, stressful situations, and hypervigilance makes it hard to “turn off.”
Insufficient Sleep Between Shifts Nurses working consecutive 12-hour shifts often experience inadequate sleep between shifts, causing cumulative fatigue, according to Nursing CE Central.
Sleep Debt Accumulation: Missing 1-2 hours of sleep per night adds up. After three consecutive shifts, you’re operating on a significant sleep deficit, impacting:
- Cognitive function
- Emotional regulation
- Immune function
- Safety (both patient care and personal well-being)
Strategies for Better Sleep
Sleep Hygiene Basics
- Blackout curtains: Essential for day-sleeping night shift nurses
- White noise machines: Block household and neighborhood sounds
- Cool room temperature: 60-67°F (15-19°C) optimal
- Consistent sleep schedule: Go to bed and wake at the same times, even on days off
Pre-Sleep Routine
- Warm shower or bath
- Avoid screens 30-60 minutes before bed
- Light stretching or gentle yoga
- Meditation or deep breathing exercises
Nutrition for Sleep
- Avoid caffeine at least 4-6 hours before sleeping
- Light post-shift meal, not heavy dinner
- Consider magnesium-rich foods (almonds, spinach, bananas)
- Avoid alcohol—it fragments sleep quality
Managing Day-Sleep for Night Shifters
- Wear sunglasses on the morning commute home
- Inform family/roommates of sleep schedule
- Silence phone notifications
- Consider melatonin supplementation (consult healthcare provider)
The Long-Term Health Impact
Chronic sleep disruption from shift work has been linked to:
- Increased cardiovascular disease risk
- Higher rates of obesity and metabolic syndrome
- Weakened immune system
- Increased cancer risk (particularly breast cancer in female night shift workers)
- Mental health challenges, including depression and anxiety
During my ICU nursing years, I witnessed colleagues develop serious health conditions directly linked to years of night shift work. This isn’t meant to scare—but rather to emphasize the importance of prioritizing sleep health as much as possible.
Transitioning Between Shifts
Rotating from Days to Nights (or Vice Versa)
- Allow 2-3 days for adjustment if possible
- Gradually shift sleep schedule by 1-2 hours daily
- Use strategic napping (20-30 minute power naps only)
- Be patient with yourself during transition periods
From personal experience, the body never fully adjusts to constant schedule changes. Your circadian rhythm can’t be reprogrammed at will—you’re asking your body to work against its fundamental biology.
Work-Life Balance: The Myth vs. Reality
The “Three Days a Week” Misconception
Let’s address this directly: working three 12-hour shifts does not automatically equal excellent work-life balance.
The Reality:
- Day 1: Work, recover, sleep
- Day 2: Work, recover, sleep
- Day 3: Work, recover, sleep
- Day 4: Deep recovery needed—often spent mostly sleeping and recuperating
- Days 5-7: Actual “free” time
You have approximately 3-4 truly free days weekly, not the mythical four days off that non-nurses imagine.
Family Life and Relationships
Missing Important Moments Nurses regularly miss:
- Children’s school events
- Family dinners
- Holidays and celebrations
- Friends’ social gatherings
- Partner’s important moments
Long shifts mean nurses may leave home before family members wake and return when young children are already in bed. During consecutive shifts, you might not see your family awake for three days straight.
The Parenting Challenge
Childcare Logistics
- Finding 12-hour childcare is expensive and challenging
- Many nursing couples work opposite shifts to avoid childcare costs (sacrificing couple time)
- School pickups become complicated
- Attending parent-teacher conferences during weekday business hours is nearly impossible.
Many RNs with young children choose night shifts to lessen childcare burdens, allowing households to split parenting responsibilities, according to Nursejournal.org.org—but this means parents rarely see each other awake.
Social Life Impact
Friendship Maintenance. Most social activities happen on weekends. Nurses work many weekends. The math creates social isolation.
From my experience, friends eventually stopped inviting me to events because I declined so frequently due to work schedules. It wasn’t personal—but the pattern damaged relationships nonetheless.
Romantic Relationships
- Dating is complicated with irregular schedules
- Exhaustion reduces quality time with partners
- Emotional depletion affects relationship engagement
- Shift work correlated with higher divorce rates among healthcare workers
Household Management
The Invisible Labor. On days off, nurses still must:
- Grocery shopping
- Meal prep for work week
- Laundry (scrubs need frequent washing)
- House cleaning
- Errands and appointments
- Bill paying and administrative tasks
These aren’t “days off”—they’re work-support days.
Exercise and Personal Health
The Irony Healthcare professionals promoting health often struggle to maintain their own:
- Fatigue and physical exertion from demanding schedules make it easier to neglect personal health
- Too exhausted to exercise after 12-hour shifts
- Meal prep feels like another chore
- Preventive healthcare appointments get postponed indefinitely
I went two years without seeing a dentist during my most intense nursing period—despite constantly educating patients about preventive care.
Financial Pressure and Side Hustles
29% of nurses reported supplementing their income with secondary sources, including working per diem (26%), non-nursing side hustles (20%), and overtime (19%), according to Nurse.org.
“Three days a week” often becomes four or five with overtime shifts, further reducing work-life balance but providing necessary income.
Mental Health and Personal Time
Self-Care Isn’t Selfish Nurses are notoriously poor at prioritizing their own well-being. The profession attracts people-pleasers and caregivers—personality traits that make self-care feel indulgent.
Reality Check: You cannot pour from an empty cup. Burned-out nurses provide suboptimal care. Prioritizing your mental health isn’t selfish—it’s essential for patient safety.
Finding Balance: Strategies That Actually Work
Boundary Setting
- Learn to say no to extra shifts (even when guilt-tripped)
- Protect days off—don’t check work emails or answer calls
- Communicate needs clearly to family and friends
Quality Over Quantity
- Focus on meaningful activities during free time
- Be fully present (not doom-scrolling or zoning out)
- Schedule specific family/friend time and protect it
Realistic Expectations
- Accept you can’t do everything
- Some weeks will be survival mode—that’s okay
- Progress, not perfection
Professional Help
- Therapy or counseling for stress management
- Marriage counseling if relationships are strained
- Financial planning to reduce money stress
[Table: Work-Life Balance Reality Check]
| Aspect | Common Perception | Actual Reality |
| Days Off | 4 full days off weekly | 3-4 days, with 1-2 spent recovering |
| Family Time | Evenings and weekends are free | Missed dinners, irregular weekends, holiday work |
| Social Life | Easy to maintain friendships | Frequent cancellations, social isolation |
| Personal Health | Healthcare workers are healthy | High rates of obesity, stress-related illness |
| Energy Levels | Free time = high energy | Often too exhausted for activities |
| Financial Stability | Good salary = comfortable living | 29% need second jobs/side hustles |
Mental Health, Burnout, and Emotional Exhaustion
The Burnout Epidemic
23% of nurses are considering leaving the profession, with RNs (23%) and LPNs/LVNs (22%) showing the highest intent to leave, according to Nurse.com. This statistic represents a crisis—not just for healthcare systems, but for the nurses suffering.
What Burnout Actually Feels Like
The World Health Organization defines burnout as chronic workplace stress that hasn’t been successfully managed, characterized by:
- Emotional exhaustion: Feeling drained, depleted, unable to give more
- Depersonalization: Becoming cynical, detached from patients and colleagues
- Reduced personal accomplishment: Feeling ineffective, doubting your competence
Burnout isn’t just feeling tired. It’s:
- Dreading work days with physical anxiety
- Crying in the bathroom during breaks
- Feeling nothing when patients share emotional moments
- Questioning whether you can continue nursing
- Experiencing compassion fatigue—inability to empathize with suffering
In 2020, nearly two-thirds of nurses (62%) experienced burnout, with 69% of nurses under 25 reporting burnout, according to the American Nurses Association.
Contributing Factors to Nurse Burnout
Understaffing and High Patient Ratios Unmanageable nurse-to-patient ratios, salary dissatisfaction, and poor leadership responsiveness negatively impact mental health, according to Nurse.com.
When one nurse cares for 8-10 patients requiring complex care, something must be sacrificed—usually thoroughness, patient education, or the nurse’s bathroom breaks.
Lack of Support: 39% of nurses didn’t feel supported by employers. When administration responds to concerns with “just work harder” or “be more grateful for your job,” it creates resentment and hopelessness.
Moral Injury. Moral injury is a psychological wound that happens when a person must take actions or witness actions that deeply violate held moral beliefs, according to the American Nurses Association.
Examples from my nursing experience:
- Knowing a patient needs closer observation, but not having time due to other critical patients
- Discharging patients who clearly need continued care due to insurance limitations
- Watching elderly patients suffer because families can’t afford hospice care
- Being forced to work mandated overtime when exhausted, knowing you’re not at your best
The Emotional Toll of Patient Care
Trauma Exposure Nurses regularly witness:
- Deaths (sometimes multiple per shift)
- Severe injuries and violence aftermath
- Child abuse cases
- End-of-life suffering
- Medical emergencies and resuscitation
In the ER, I’ve held dying patients’ hands when no family could be reached. I’ve performed CPR knowing it was futile. I’ve cleaned and prepared the bodies of people who were laughing hours earlier. This emotional weight accumulates.
Compassion Fatigue: The cost of caring. After years of absorbing others’ trauma, pain, and grief, nurses can become emotionally numb as a protective mechanism.
Workplace Violence and Verbal Abuse
Acute care nurses were significantly more likely to experience verbal abuse, intimidation, or physical assault by patients, patients’ family members, or colleagues, according to Nurse.com.
Being punched, kicked, spit on, verbally abused—these aren’t rare occurrences. They’re normalized aspects of nursing that shouldn’t be.
The Stress-Burnout-Departure Cycle
More than 138,000 nurses have left the workforce since 2022, reporting stress, burnout, and retirement as key reasons, according to the National Council of State Boards of Nursing. Approximately 40% of nurses plan to leave nursing within the next five years Advisory.
This creates a vicious cycle:
- Nurses leave due to burnout
- Remaining nurses face higher workloads
- Increased workload accelerates burnout
- More nurses leave
- Cycle repeats
Mental Health Statistics
Depression and Anxiety Studies show 30-40% of nurses experience depression or anxiety symptoms, significantly higher than the general population.
Substance Abuse Nurses have higher rates of substance use disorders than the general population, partly due to stress and easy medication access.
Suicide Risk Female nurses face increased suicide risk compared to other professions—a sobering statistic that demands attention.
Stigma Around Mental Health in Nursing
The culture of nursing often promotes a “tough it out” mentality. Admitting struggles feels like admitting weakness. Many nurses fear:
- Judgment from colleagues
- Being perceived as incompetent
- Licensing board investigations if seeking mental health treatment
- Job loss or career damage
This stigma prevents nurses from seeking desperately needed help.
Coping Mechanisms: Healthy and Unhealthy
Unhealthy Coping (Common but Destructive):
- Alcohol use to “decompress.”
- Emotional eating
- Social withdrawal and isolation
- Medication misuse
- Ignoring problems until the crisis point
Healthy Coping Strategies:
- Professional counseling or therapy
- Peer support groups
- Mindfulness and meditation practices
- Physical activity and exercise
- Creative outlets (art, music, writing)
- Setting firm boundaries between work and personal life
Getting Help: Resources for Nurses
Employee Assistance Programs (EAP) Most hospitals offer confidential counseling services—use them without shame.
Professional Organizations
- American Nurses Association (ANA) Healthy Nurse, Healthy Nation program
- National Council of State Boards of Nursing peer assistance programs
- State nursing associations with mental health resources
Crisis Resources
- National Suicide Prevention Lifeline: 988
- Crisis Text Line: Text HOME to 741741
- SAMHSA National Helpline: 1-800-662-4357
Organizational Solutions Needed
Individual coping strategies help, but systemic problems require systemic solutions:
- Safe nurse-to-patient ratios are mandated by law
- Mental health support integrated into workplace culture
- Leadership training emphasizing staff wellbeing
- Fair compensation reflecting work demands
- Adequate time off between shifts
- Zero-tolerance policies for workplace violence
From my experience, healthcare organizations that genuinely prioritize nurse wellbeing—not just with empty slogans but with concrete actions and resources—retain staff and provide better patient care.
Financial Reality: Salary, Benefits, and Side Hustles
Salary Expectations Across the United States
Nurse salaries vary significantly based on location, specialty, experience, and education level.
National Averages (2024 Data):
- Registered Nurse (RN) median salary: $81,220 annually
- Licensed Practical Nurse (LPN): $54,620 annually
- Nurse Practitioner (NP): $121,610 annually
Regional Variations:
- California: $124,000 – highest paying state
- New York: $96,000
- Texas: $77,000
- Florida: $72,000
- Rural Midwest: $62,000 – $70,000
These figures represent base pay before taxes, insurance, retirement contributions, and student loan payments.
The Real Take-Home Reality
Let’s break down a typical RN salary in a mid-cost area:
- Gross annual salary: $75,000
- Federal taxes (22% bracket): -$16,500
- State taxes (avg 5%): -$3,750
- Social Security/Medicare: -$5,738
- Health insurance premiums: -$4,800 annually
- Retirement contribution (6%): -$4,500
- Student loan payment: -$6,000 annually
Net annual income: Approximately $33,712. Monthly take-home: Around $2,809
This explains why 29% of nurses supplement their income despite earning “decent” salaries on paper.
Student Loan Burden
The Investment:
- Associate’s Degree in Nursing (ADN): $6,000 – $40,000
- Bachelor of Science in Nursing (BSN): $40,000 – $100,000+
- Master of Science in Nursing (MSN): Additional $40,000 – $70,000
- Doctor of Nursing Practice (DNP): Additional $50,000 – $120,000
Many nurses carry $50,000 – $100,000 in student loan debt, with monthly payments of $500 – $1,000 consuming significant portions of take-home pay.
The Side Hustle Reality
Nurses supplement income through per diem work (26%), non-nursing side hustles (20%), and overtime (19%).
Popular Nurse Side Hustles:
- Per diem hospital shifts: Work extra shifts at higher hourly rates (no benefits)
- Travel nursing: Temporary contracts in high-need areas (significantly higher pay but unstable)
- Telehealth nursing: Remote patient consultations
- Nursing education: Teaching CPR, first aid, or nursing courses
- Medical writing: Creating healthcare content for websites and publications
- Legal nurse consulting: Assisting law firms with medical cases
- Corporate wellness programs: Workplace health screening and education
Non-Nursing Side Hustles:
- Freelance writing or blogging
- Real estate
- Online tutoring
- E-commerce or Etsy shops
- Rideshare driving (though questionable after 12-hour shifts)
The irony isn’t lost: nurses work physically and emotionally demanding 36-40 hour workweeks, then work additional hours just to achieve financial stability.
Benefits: The Hidden Compensation
Healthcare Benefits Most hospitals offer health insurance, though:
- Premiums average $400-600 monthly for family coverage
- High deductibles ($3,000-$6,000) mean high out-of-pocket costs
- Dental and vision often require separate premiums
Retirement Benefits
- 401(k) matching: Typically 3-6% employer match
- Pension plans: Rare, but some government and union positions offer them
- 403(b) plans: Common in nonprofit hospitals
Other Benefits:
- Paid time off (PTO): 2-4 weeks annually for new nurses, increasing with seniority
- Continuing education allowances
- Tuition reimbursement programs
- Shift differentials (night shift typically adds $3-8/hour)
- Weekend differentials (additional $2-5/hour)
Career Advancement and Salary Growth
Experience-Based Increases:
- 0-2 years: Base salary
- 3-5 years: 10-15% increase
- 6-10 years: 20-30% increase
- 10+ years: 30-50% increase
Specialization Premium:
- ICU/Critical Care: +10-20% above med-surg
- Emergency Department: +15-20%
- Operating Room: +15-25%
- Labor & Delivery: +10-15%
- Travel Nursing: +50-100% (but temporary and no benefits)
Advanced Degrees:
- BSN vs ADN: $5,000-10,000 annual increase
- MSN (Nurse Practitioner): $40,000-60,000 increase over RN salary
- DNP: Additional $10,000-20,000 over MSN
Geographic Arbitrage
Some nurses strategically relocate for better compensation:
- Moving from low-cost, low-wage areas to high-cost, high-wage areas can significantly improve purchasing power if expenses are managed carefully
- Travel nursing in high-need areas can earn $100,000-150,000 annually with housing stipends
Union vs. Non-Union Positions
Union Benefits:
- Negotiated pay scales with guaranteed increases
- Stronger protections against unfair practices
- Better benefits packages
- Enforceable staffing ratios (in some states)
Non-Union Reality:
- Pay increases at the employer’s discretion
- Fewer protections
- Often lower benefits
- More vulnerable to sudden policy changes
The Golden Handcuffs Phenomenon
Despite financial stress, leaving nursing feels impossible when:
- Student loans require consistent income
- Health insurance is employer-tied
- Family depends on your salary
- You’ve invested years in this career path
Many nurses feel trapped—burned out but financially unable to leave or transition careers.
Financial Wellness Strategies for Nurses
Budgeting Essentials:
- Track every expense for one month
- Identify areas for reduction
- Build an emergency fund (3-6 months’ expenses)
- Automate savings before spending
Debt Payoff Strategies:
- Public Service Loan Forgiveness (PSLF) for qualifying nonprofit hospital employees
- Income-driven repayment plans for federal loans
- Aggressively pay off high-interest private loans first
- Refinancing when interest rates are favorable
Investment Priorities:
- Employer 401(k) match (free money)
- High-interest debt payoff
- Emergency fund
- Additional retirement contributions (Roth IRA)
- Other investment vehicles
Increasing Income:
- Negotiate salary during hiring and performance reviews
- Obtain specialty certifications
- Pursue advanced degrees strategically
- Consider per diem work at higher hourly rates
- Develop passive income streams
[Table: Nursing Salary by Specialty (2024 US Averages)]
| Specialty | Average Annual Salary | Typical Education | Certification Required |
| Nurse Practitioner | $121,610 | MSN/DNP | Yes |
| Nurse Anesthetist | $203,090 | Master’s/Doctorate | Yes |
| Nurse Midwife | $114,210 | Master’s | Yes |
| Clinical Nurse Specialist | $84,060 | MSN | Often |
| ICU/Critical Care RN | $88,000 | BSN preferred | Recommended |
| Emergency Room RN | $86,000 | BSN preferred | ACLS/PALS |
| Operating Room RN | $85,000 | BSN preferred | CNOR recommended |
| Labor & Delivery RN | $82,000 | BSN preferred | Specialty cert |
| Medical-Surgical RN | $75,000 | ADN/BSN | Basic RN license |
| Long-Term Care RN | $71,000 | ADN/BSN | Basic RN license |
Different Settings, Different Lifestyles
Hospital Nursing: The Traditional Path
Inpatient Medical-Surgical Units
- 12-hour rotating shifts (days/nights/weekends)
- Patient ratios: 5-7 patients per nurse
- Moderate to high stress
- Predictable (yet unpredictable) environment
- Best for: New graduates building fundamental skills
Intensive Care Units (ICU)
- 12-hour shifts with high intensity
- Patient ratios: 1-2 patients per nurse
- High stress, high acuity
- Significant overtime common
- Best for: Nurses who thrive on critical thinking and emergencies
Emergency Department
- 8-12 hour shifts, high variability
- Patient volume fluctuates wildly
- Extreme stress during “surge” periods
- Fast-paced, never boring
- Best for: Adrenaline junkies who love variety
Operating Room
- Typically Monday-Friday, 8-10 hour shifts (elective surgeries)
- On-call requirements for emergencies
- Lower patient ratios but high technical demands
- Better work-life balance than floor nursing
- Best for: Nurses preferring technical precision over bedside care
Labor & Delivery
- 12-hour shifts with unpredictable workload
- Beautiful moments mixed with emotional tragedy
- On-call requirements common
- Patient ratios vary significantly
- Best for: Nurses drawn to maternal-child health
From my hospital experience across ER, Pediatrics, ICU, and General Wards, each setting demands different stamina. The ER taught me rapid assessment and crisis management. ICU required meticulous attention to detail and comfort with technology. Pediatrics demanded patience, creativity, and family-centered communication.
Outpatient and Clinic Nursing
Physician Office Nursing
- Monday-Friday, 8-5 PM, typical schedule
- No nights, weekends, or holidays
- Lower stress compared to hospitals
- More predictable patient flow
- Lower salary (typically 10-20% less than hospital)
- Best for: Nurses prioritizing work-life balance and routine
Ambulatory Surgery Centers
- Day shifts only, minimal weekends
- Pre-op and post-op care focus
- Moderate stress level
- Predictable schedule
- Best for: OR nurses wanting better hours
Dialysis Centers
- Typically Monday-Friday or Tuesday-Saturday
- Consistent patient population
- Routine-focused with occasional emergencies
- Building long-term patient relationships
- Best for: Nurses who value patient continuity
Many nurses with young children choose roles with more predictable hours in outpatient settings, accepting lower pay for a better quality of life.
Specialized Hospital Departments
Pediatrics
- Similar hours to general hospital nursing
- Requires patience with pediatric patients and anxious parents
- Emotionally rewarding but also heartbreaking
- Play therapy and distraction techniques are essential
- Best for: Nurses passionate about children’s health
Psychiatric/Mental Health
- 8-12-hour shifts, depending on facility
- Higher risk of violence than in general nursing
- Requires strong de-escalation skills
- Emotionally demanding is different from medical nursing
- Best for: Nurses interested in behavioral health
Hospice and Palliative Care
- Variable schedules, often on-call
- Home visits or inpatient hospice facilities
- Emotionally profound work
- Requires comfort with death and dying
- Best for: Compassionate nurses wanting meaningful end-of-life care
Non-Traditional Nursing Careers
School Nursing
- School hours and calendar (summers off!)
- Lower stress, more autonomous
- Focus on wellness and prevention
- Significant pay cut from hospital nursing
- Best for: Nurses with children who want aligned schedules
Occupational/Corporate Health Nursing
- Business hours only
- Employee wellness programs, injury management
- Lower stress environment
- Requires a different skill set
- Best for: Nurses wanting traditional work hours
Public Health Nursing
- Variable schedules, often business hours
- Community education and prevention focus
- Less hands-on medical care
- Population health approach
- Best for: Nurses interested in broader health impact
Telehealth/Remote Nursing
- Work from home
- Phone or video consultations
- Growing field post-COVID
- Requires strong communication skills
- Best for: Nurses seeking location flexibility
Travel Nursing
- 13-week temporary contracts nationwide
- Significantly higher pay ($2,000-4,000+ weekly)
- Housing stipends and benefits
- Constant relocation and adaptation
- No job security between contracts
- Best for: Adventurous nurses without strong geographic ties
Per Diem/Agency Nursing
- Work on-demand at various facilities
- Highest hourly rates
- No guaranteed hours or benefits
- Maximum schedule flexibility
- Best for: Experienced nurses wanting control over schedules
Nurse Educator
- Teaching in nursing programs
- Typically requires a Master’s degree
- Academic calendar with summers lighter
- Significantly lower pay than clinical nursing
- Best for: Nurses passionate about education and shaping future nurses
Legal Nurse Consultant
- Assisting law firms with medical cases
- Business hours
- Requires clinical expertise and analytical skills
- Variable income based on case load
- Best for: Detail-oriented nurses interested in legal aspects
Lifestyle Comparison
[Table: Nursing Settings Lifestyle Comparison]
| Setting | Typical Schedule | Stress Level | Work-Life Balance | Pay Range | Best Aspect | Worst Aspect |
| Hospital Med-Surg | 12-hr rotating shifts | High | Poor-Fair | $$ | Skill variety | Exhausting, weekends/holidays |
| ICU | 12-hr rotating shifts | Very High | Poor | $$$ | Critical thinking | Emotional toll, high acuity |
| Emergency Dept | 8-12 hr shifts | Very High | Fair | $$$ | Fast-paced variety | Unpredictable, violence risk |
| Operating Room | 8-10 hr, M-F + call | Moderate | Good | $$$ | Technical skills | On-call requirements |
| Clinic/Office | 8-5, M-F | Low-Moderate | Excellent | $-$$ | Predictable hours | Lower pay, routine work |
| School Nursing | School hours | Low | Excellent | $ | Summers off, autonomy | Significant pay cut |
| Travel Nursing | 12-hr, 13-week contracts | High | Poor-Good | $$$$ | High pay, adventure | Constant relocation, unstable |
| Telehealth | Varies, remote | Low-Moderate | Excellent | $-$$ | Work from home | Limited hands-on care |
| Hospice | Variable, on-call | Moderate-High | Fair | $$ | Meaningful work | Emotional weight |
Choosing the Right Setting for Your Life Stage
New Graduates (0-2 years): Hospital settings provide essential skill development despite demanding schedules. Build foundational competencies before specializing.
Nurses with Young Children: Outpatient settings, school nursing, or night shifts (if partner works days) often work better than rotating hospital schedules.
Mid-Career (5-10 years): Specialization opportunities open up. Consider certifications, advanced degrees, or transitioning to preferred settings.
Late Career (15+ years): Many experienced nurses transition to less physically demanding roles—education, administration, case management, or consulting.
Pre-Retirement: Per diem or part-time positions allow a gradual reduction of work hours while maintaining income and benefits.
From my own career trajectory, I’ve found that matching your nursing specialty to your current life circumstances significantly impacts job satisfaction and sustainability. What works at age 25 may be unbearable at 45 with family obligations.
Strategies for Sustainable Nursing: Making It Work Long-Term
Physical Sustainability
Body Mechanics and Injury Prevention
- Always use proper lifting techniques (even when rushed)
- Utilize patient lifts and transfer equipment—never too busy to use safety devices
- Invest in high-quality compression stockings
- Wear proper, supportive shoes designed for healthcare workers
- Stretch before, during, and after shifts
Physical Exercise Despite physically demanding work, nurses must maintain additional exercise for overall health. Nursing involves specific muscle groups repeatedly; balanced exercise prevents overuse injuries.
Recommended Activities:
- Low-impact cardio (swimming, cycling) to protect joints
- Yoga or Pilates for core strengthening and flexibility
- Strength training for injury prevention
- Walking on non-work days
Listen to Your Body. Early signs of physical breakdown:
- Persistent back, knee, or foot pain
- Chronic fatigue that doesn’t improve with rest
- Frequent illness due to weakened immunity
- Sleep disturbances
Ignoring these signs leads to serious long-term health consequences. From experience, nurses often push through pain until forced to stop—preventive care is cheaper and less painful than intervention after injury.
Mental and Emotional Sustainability
Establishing Boundaries
- Say no to guilt-tripping about extra shifts
- Don’t check work messages on days off
- Limit work discussion during personal time
- Protect vacation time—actually take vacations
Decompression Rituals Create consistent post-shift rituals signaling work-mode to home-mode transition:
- Shower immediately upon arriving home
- Change into comfortable clothes
- Brief meditation or deep breathing
- Light walk or gentle stretching
- Avoid immediately discussing difficult cases (unless processing is needed)
Regular Mental Health Check-Ins
- Therapy or counseling (preventive, not just crisis intervention)
- Journaling to process experiences
- Peer support groups
- Mindfulness or meditation practices
Compassion Fatigue Prevention
- Recognize early warning signs (cynicism, emotional numbness)
- Take mental health days when needed
- Engage in activities completely unrelated to nursing
- Maintain identity beyond “nurse.”
Professional Sustainability
Continuing Education
- Maintain certifications and licenses
- Pursue specialty certifications aligned with interests
- Attend conferences and workshops
- Stay current with evidence-based practices
Career Development
- Set professional goals beyond bedside nursing if desired
- Consider advancement opportunities (charge nurse, management, education)
- Develop niche expertise valuable to employers
- Build a professional network
Finding Meaning in Work Nurses who feel their work has meaning and purpose are less likely to experience burnout.
Ways to maintain purpose:
- Remember why you chose nursing
- Focus on small victories and positive patient interactions
- Mentor new nurses
- Participate in quality improvement initiatives
- Advocate for patients and the profession
Know When to Change Sometimes the solution isn’t adjusting your current position—it’s finding a better fit:
- Different specialty
- Different facility
- Different shift
- Different nursing role entirely
I’ve changed specialties multiple times throughout my career. Each transition revitalized my passion for nursing when I felt stagnant or burned out.
Financial Sustainability
Living Below Your Means
- Don’t fall into lifestyle inflation with salary increases
- Maintain an emergency fund for job transitions
- Pay down high-interest debt aggressively
- Save for retirement consistently
Strategic Career Moves
- Negotiate salary during hiring and reviews
- Pursue certifications that command premium pay
- Consider travel contracts strategically
- Develop multiple income streams
Plan for Long-Term Nursing is physically demanding—plan for career longevity:
- Transition to less physically demanding roles with age
- Invest in retirement aggressively in an early career
- Develop skills transferable beyond bedside nursing
Building Resilience
Social Support Networks
- Connect with other nurses who understand the reality
- Maintain friendships outside healthcare
- Nurture family relationships despite schedule challenges
- Consider therapy or support groups
Stress Management Techniques
- Deep breathing exercises during the shift
- Brief meditation (even 5 minutes helps)
- Progressive muscle relaxation
- Cognitive reframing of stressors
Joy and Humor Healthcare is serious, but humor provides necessary relief. Dark humor among healthcare workers isn’t callousness—it’s a survival mechanism. Finding moments of lightness prevents drowning in heaviness.
Advocacy and Systemic Change
Individual nurses cannot fix broken systems alone, but collective action creates change:
- Join professional nursing organizations
- Support unionization efforts where appropriate
- Advocate for safe staffing ratios
- Report unsafe conditions through proper channels
- Vote for candidates supporting healthcare workers
- Share your story to educate the public and legislators
Speaking Up
- Report unsafe practices
- Advocate for patient safety
- Demand adequate resources
- Support colleagues experiencing difficulties
Knowing When to Leave
Sometimes the healthiest choice is leaving nursing—and that’s okay.
Signs it might be time:
- Physical health deteriorating despite interventions
- Persistent depression, anxiety, or substance dependence
- Inability to provide safe patient care
- Feeling trapped with no hope for improvement
- Dreading work to the point of physical illness
Nursing shouldn’t cost you your health, relationships, or life. Your worth isn’t defined by this profession.
Alternative Careers for Experienced Nurses
Within Healthcare:
- Healthcare administration
- Quality improvement specialist
- Infection control
- Case management
- Health insurance review
- Medical sales
- Pharmaceutical research
Outside Healthcare:
- Medical writing and journalism
- Healthcare consulting
- Health technology companies
- Teaching (non-nursing subjects)
- Entrepreneurship using healthcare knowledge
The Long View
A sustainable nursing career spans 30-40 years. It’s a marathon, not a sprint. Strategies working in year two may be unsustainable by year ten. Continuously reassess and adjust.
From my decade in nursing, I’ve learned that flexibility and self-awareness are crucial. Listen to your body, honor your mental health, and remember that you deserve a life beyond nursing.
Acknowledgments
I would like to thank my colleagues across the emergency, pediatric, intensive care, and general ward nursing departments who have shared their experiences and insights throughout my nursing career. Their perspectives have enriched this article and reminded me that nurses’ daily realities, while challenging, are also filled with profound meaning and impact.
Special appreciation to the Ghana Health Service for providing the clinical environment where I developed the expertise informing this work, and to my fellow members of the Ghana Registered Nurses and Midwives Association (GRNMA) for their continued support and professional development opportunities.
Thanks also to the nursing community worldwide, who openly share their stories online, helping break down the romanticized misconceptions about nursing and allowing aspiring nurses to make informed career decisions.
Finally, gratitude to the readers of Muminmed.com who engage with evidence-based healthcare content and support nurses through understanding the reality of our profession.
Frequently Asked Questions (FAQs)
Q: What does a typical day look like for a hospital nurse?
A: A typical 12-hour hospital shift involves arriving 15 minutes early (unpaid) to review patient charts, receiving handoff report from the previous shift, conducting initial patient assessments, administering multiple medication rounds throughout the day, performing procedures and treatments, managing emergencies or admissions, extensive documentation, and reporting to the incoming shift—often staying 30-60 minutes late to complete charting. Actual patient care time is interspersed with administrative tasks, family communication, and multitasking between multiple patients’ needs. Most nurses walk 4-5 miles per shift and rarely get uninterrupted breaks.
Q: Do nurses really only work three days per week?
A: While many nurses work three 12-hour shifts weekly (36 hours), this doesn’t translate to “only” three days of work. Each 12-hour shift requires preparation time (1-2 hours), post-shift recovery time (3-4 hours), and adequate sleep (8-10 hours), meaning each workday effectively consumes 24-28 hours of your life. The day following three consecutive shifts is typically spent recovering from exhaustion. Additionally, 29% of nurses work overtime or second jobs to supplement income, further reducing the perceived “four days off” advantage.
Q: How do nurses handle working night shifts?
A: Night shift nursing involves sleeping during daytime hours, which fights natural circadian rhythms and never feels fully natural to most nurses. Strategies include blackout curtains, white noise machines, establishing consistent sleep schedules, wearing sunglasses during morning commutes home, and strategic use of caffeine limited to the first half of the shift. Despite these adaptations, night shift work is associated with sleep quality issues, increased health risks, and social isolation. Many nurses rotate between day and night shifts, which is even more disruptive to the body’s natural rhythms.
Q: What is nurse burnout, and how common is it?
A: Nurse burnout is chronic workplace stress characterized by emotional exhaustion, depersonalization (becoming cynical toward patients), and a reduced sense of accomplishment. Research shows 62% of nurses experienced burnout in 2020, with 69% of nurses under age 25 reporting burnout. Contributing factors include understaffing, unmanageable patient ratios, lack of administrative support, moral injury from witnessing care they know is inadequate, exposure to trauma, and insufficient recovery time between demanding shifts. Burnout has driven 23% of nurses to consider leaving the profession entirely.
Q: How do nurses maintain work-life balance?
A: Honest answer: Most struggle significantly with work-life balance. Long 12-hour shifts mean missing family dinners, children’s activities, social events, and holidays. Exhaustion on work days limits quality time with loved ones. Strategies that help include setting firm boundaries about extra shifts, protecting days off from work intrusion, scheduling specific family time and treating it as non-negotiable, choosing nursing specialties with more predictable schedules (like clinic nursing), and accepting that some weeks will be survival mode rather than perfect balance. Many nurses sacrifice career advancement to prioritize personal life.
Q: What should nurses eat during 12-hour shifts to maintain energy?
A: Optimal shift nutrition includes planning at least one main meal and two snacks with balanced macronutrients. Focus on complex carbohydrates for sustained energy (quinoa, brown rice, sweet potatoes), lean proteins for muscle repair and satiety (chicken, fish, eggs, Greek yogurt), healthy fats for brain function (avocados, nuts, olive oil), and plenty of vegetables and fruits for vitamins and fiber. Pack meals in advance because cafeteria options are often unhealthy and expensive. Aim for 2-3 liters of water per shift, and limit caffeine to the first 4-6 hours of your shift to avoid sleep disruption afterward. Avoid sugary snacks that cause energy crashes.
Q: How much do nurses really make after taxes and expenses?
A: While the median RN salary is approximately $81,220 nationally, actual take-home pay is significantly less. After federal taxes (22% bracket), state taxes, Social Security/Medicare, health insurance premiums, retirement contributions, and student loan payments, a nurse earning $75,000 gross might take home only $33,000-40,000 annually (around $2,800-3,300 monthly). This explains why 29% of nurses work second jobs or overtime despite “decent” salaries on paper. Geographic location dramatically affects purchasing power—California pays the highest, but has an extreme cost of living, while rural areas pay less, but expenses are lower.
Q: What are the best nursing specialties for a better lifestyle?
A: Nursing specialties with better work-life balance typically include clinic or office nursing (Monday-Friday, 8-5 PM schedules), school nursing (aligned with school calendar, including summers off), occupational health nursing (business hours), and ambulatory surgery centers (minimal weekends). These positions usually offer more predictable schedules and lower stress, but often come with 10-20% pay cuts compared to hospital nursing. Within hospitals, operating room nursing often has better schedules for elective procedures, though on-call requirements apply. The trade-off is almost always predictable hours versus higher pay and more acute care.
Q: How physically demanding is nursing really?
A: Nursing is extremely physically demanding—comparable to manual labor professions. Nurses walk 4-5 miles per shift (10,000-12,000 steps), lift or reposition patients weighing 100-300 pounds multiple times, stand for 8-10 hours of 12-hour shifts, and perform repetitive motions constantly. This leads to high rates of back injuries, knee and foot problems, varicose veins from prolonged standing, and musculoskeletal disorders. Studies show 60-80% of nurses experience lower back pain at some point. Unlike traditional labor jobs, nursing combines this physical demand with critical thinking, emotional labor, and high-stress decision-making simultaneously.
Q: Can you raise a family while working as a nurse?
A: Yes, but it requires significant planning, support systems, and often sacrifices. Challenges include finding 12-hour childcare (expensive and limited), missing children’s activities due to shift work, working holidays and weekends, and being too exhausted for quality family time on work days. Many nursing couples work opposite shifts to reduce childcare costs, which means they rarely see each other. Some nurses choose night shifts to be home during children’s waking hours, sacrificing their own sleep. Outpatient nursing positions with regular business hours offer better family compatibility but lower salaries. Single-parent nurses face particularly intense challenges.
Q: What resources exist for nurses experiencing mental health struggles?
A: Multiple resources support nurses’ mental health: Employee Assistance Programs (EAP) through most hospitals offer confidential counseling, the American Nurses Association’s Healthy Nurse, Healthy Nation program provides wellness resources, state nursing boards often have peer assistance programs for nurses struggling with substance use or mental health issues, and professional organizations offer support groups. Crisis resources include the National Suicide Prevention Lifeline (988), Crisis Text Line (text HOME to 741741), and SAMHSA National Helpline (1-800-662-4357). Reducing stigma around seeking help is crucial—mental health struggles don’t indicate weakness or incompetence.
Q: Is it worth becoming a nurse, given all these challenges?
A: This depends entirely on individual values, priorities, and circumstances. Nursing offers job security, meaningful work, diverse specialization options, geographic flexibility, and decent income potential. However, it demands significant physical stamina, emotional resilience, schedule flexibility, and personal sacrifice. The profession faces serious systemic problems, including understaffing, burnout, and inadequate support that won’t resolve quickly. Before entering nursing, honestly assess your tolerance for shift work, physical demands, emotional labor, and work-life balance challenges. Shadow working nurses across multiple settings to observe reality beyond romanticized portrayals. Nursing can be profoundly rewarding, but it’s not for everyone—and that’s perfectly acceptable.
Conclusion
The realistic daily lifestyle of working nurses bears little resemblance to the sanitized, inspiring television portrayals most people encounter. It’s not just long shifts—it’s the cumulative physical exhaustion, emotional depletion, disrupted circadian rhythms, strained relationships, and constant feeling that you’re giving everything, yet it’s never quite enough.
This reality check isn’t meant to discourage aspiring nurses or diminish the profound meaning many find in this profession. Rather, it’s about entering nursing with eyes wide open, making informed decisions about specialties and settings, and developing sustainable strategies from day one rather than burning out and leaving the profession entirely.
From my 10 years across emergency, pediatric, intensive care, and general ward nursing with the Ghana Health Service, I’ve experienced the full spectrum—the incredible satisfaction of saving lives, the heartbreak of losing patients despite best efforts, the camaraderie among colleagues facing impossible situations together, and the frustration with systems that demand more than humans can reasonably give.
If you’re currently a nurse struggling with these realities, know you’re not alone. Nearly every nurse experiences periods of questioning whether they can continue. Prioritize your health, establish firm boundaries, seek support without shame, and remember that leaving nursing doesn’t equal failure—it might be the healthiest choice.
If you’re considering nursing, ask yourself honestly: Can I handle irregular schedules, physical demands comparable to athletic training, emotional labor of witnessing suffering repeatedly, and potential sacrifice of traditional work-life balance? If yes, nursing offers incredible opportunities for impact, growth, and professional satisfaction despite its challenges.
The nursing profession desperately needs systemic change—safe staffing ratios, better mental health support, fair compensation, and cultures that prioritize nurse wellbeing alongside patient care. Individual coping strategies help, but they cannot fix broken systems. Advocacy, unionization, and collective action remain essential for creating sustainable nursing careers.
Ultimately, the realistic look at nurses’ daily lives reveals dedicated professionals navigating extraordinarily demanding circumstances to provide essential care. They deserve recognition not just during crises or appreciation weeks, but through concrete actions that support their health, safety, and sustainability throughout their entire careers.
Medical Disclaimer: This article is for informational purposes only and does not constitute medical or professional career advice. Abdul-Muumin Wedraogo is a Registered General Nurse sharing insights based on clinical experience, but individual circumstances vary significantly. Those experiencing serious mental health concerns should consult healthcare providers immediately. Career decisions should consider personal circumstances, financial situations, and individual capabilities. Always consult with career counselors, nursing educators, or experienced nurses in your specific area before making major professional decisions.
References
- American Nurses Association. (2024). Nursing workforce statistics. Retrieved from https://www.nursingworld.org/practice-policy/workforce/
- Bureau of Labor Statistics, U.S. Department of Labor. (2024). Occupational outlook handbook: Registered nurses. Retrieved from https://www.bls.gov/ooh/healthcare/registered-nurses.htm
- Dyrbye, L. N., Shanafelt, T. D., Sinsky, C. A., Cipriano, P. F., Bhatt, J., Ommaya, A., West, C. P., & Meyers, D. (2017). Burnout among health care professionals: A call to explore and address this underrecognized threat to safe, high-quality care. NAM Perspectives. https://doi.org/10.31478/201707b
- Kelly, L. A., Gee, P. M., & Butler, R. J. (2021). Impact of nurse burnout on organizational and position turnover. Nursing Outlook, 69(1), 96-102. https://doi.org/10.1016/j.outlook.2020.06.008
- National Academy of Medicine. (2019). Taking action against clinician burnout: A systems approach to professional well-being. National Academies Press. https://doi.org/10.17226/25521
- Occupational Safety and Health Administration (OSHA). (2024). Healthcare workers: Protecting healthcare workers. U.S. Department of Labor. Retrieved from https://www.osha.gov/healthcare-workers
- Substance Abuse and Mental Health Services Administration. (2023). Key substance use and mental health indicators in the United States. U.S. Department of Health and Human Services. Retrieved from https://www.samhsa.gov/data/
- Smiley, R. A., Allgeyer, R. L., Shobo, Y., Lyons, K. C., Letourneau, R. M., Zhong, E., Kamau, P. W., Lekway, I. R., & Alexander, M. (2023). The 2022 National Nursing Workforce Survey. Journal of Nursing Regulation, 14(1), S1-S90. https://doi.org/10.1016/S2155-8256(23)00047-9
- American Association of Colleges of Nursing. (2024). Nursing shortage fact sheet. Retrieved from https://www.aacnnursing.org/news-data/fact-sheets/nursing-shortage
- World Health Organization. (2020). State of the world’s nursing 2020: Investing in education, jobs and leadership. Geneva: World Health Organization. Retrieved from https://www.who.int/publications/i/item/9789240003279
About the Author
Abdul-Muumin Wedraogo, RGN, BSN, is a Registered General Nurse with over 10 years of clinical experience across Emergency, Pediatric, Intensive Care, and General Ward settings with the Ghana Health Service. He holds a Bachelor of Science in Nursing from Valley View University and graduated from Premier Nurses’ Training College, Ghana.
Abdul-Muumin is a certified member of the Nurses and Midwifery Council (NMC), Ghana, and the Ghana Registered Nurses and Midwives Association (GRNMA). Throughout his career, he has witnessed firsthand the realities of nursing life—from the exhilaration of saving lives in the Emergency Department to the profound exhaustion of consecutive 12-hour shifts, from the heartbreak of pediatric losses to the satisfaction of ICU patient recoveries.
Beyond clinical nursing, Abdul-Muumin brings technology expertise to healthcare, holding a Diploma in Network Engineering and an Advanced Professional certification in System Engineering. This unique combination allows him to evaluate medical devices and health technology from both clinical and technical perspectives.
At Muminmed.com, Abdul-Muumin provides evidence-based reviews of medical devices, smart health technology, nutritional supplements, and medical lifestyle products. His mission is to bridge the gap between clinical nursing expertise and consumer health product evaluation, helping readers make informed decisions about their health investments.
Abdul-Muumin’s writing reflects his core belief that healthcare professionals have a responsibility to educate beyond clinical settings—empowering individuals with accurate, accessible health information while respecting the complexity of medical science.








