Discover evidence-based strategies for achieving work-life balance as a registered nurse, from shift management to self-care. Expert insights from a 10-year nursing veteran.
Introduction
Recent workforce surveys show that over twenty percent of registered nurses work between 41 and 50 hours weekly, according to the Oncology Nursing Society, with many experiencing emotional exhaustion that threatens both their well-being and patient care quality. If you’ve ever finished a grueling 12-hour shift only to realize you haven’t eaten properly, missed your child’s school event, or feel too drained to enjoy your days off, you’re not alone. The struggle to maintain balance between professional responsibilities and personal life has become one of nursing’s most pressing challenges.
As Abdul-Muumin Wedraogo, a Registered General Nurse with over ten years of clinical experience across Emergency, Pediatric, Intensive Care, and General Ward settings, I’ve witnessed firsthand how the demanding nature of nursing can impact every aspect of life. Throughout my decade in healthcare, I’ve learned that achieving work-life balance as a registered nurse isn’t about perfection—it’s about creating sustainable strategies that protect your health while allowing you to provide exceptional patient care.
This comprehensive guide explores realistic work-life balance in the nursing profession, offering evidence-based strategies drawn from current research and practical clinical experience. Whether you’re a new graduate struggling with shift work or an experienced nurse seeking to recalibrate your priorities, you’ll discover actionable approaches to maintaining a healthy balance during shift work while thriving in your nursing career.
Disclosure: This article contains affiliate links. As an Amazon Associate and affiliate partner of various medical device retailers, Muminmed.com earns from qualifying purchases. This comes at no additional cost to you and helps support our work in providing evidence-based health information. All recommendations are based on clinical experience and research.
Table of Contents
Understanding Work-Life Balance in Modern Nursing
Work-life balance represents the proportion of time dedicated to professional duties compared with time spent with family and pursuing enjoyable activities, according to the American Nurse Journal. For nurses, this concept takes on unique complexity due to the unpredictable, emotionally demanding, and physically exhausting nature of healthcare work.
What Balanced Life Looks Like for Nurses
A balanced lifestyle for full-time nurses doesn’t mean equal distribution of hours between work and personal life—such a perfect equilibrium rarely exists in healthcare. Instead, it encompasses:
- Energy Management: Having sufficient physical and emotional reserves after shifts to engage meaningfully with family and personal interests
- Boundary Protection: Clear separations between professional responsibilities and personal time
- Fulfillment: Experiencing satisfaction in both career achievements and personal life pursuits
- Sustainable Practices: Maintaining health habits that support long-term career longevity
- Flexibility: Adapting to the dynamic demands of nursing while preserving core personal values
The Pendulum Approach to Balance
Rather than viewing work-life balance as a binary scale, experts consider it more like a pendulum constantly swinging between different areas of focus, according to the Oncology Nursing Society. This perspective acknowledges that balance for healthcare professionals isn’t static—some weeks require more professional dedication during crises, while other periods allow greater personal focus.
From my experience in emergency and intensive care settings, I’ve observed that nurses who successfully maintain balance understand this fluidity. They recognize that working three consecutive 12-hour shifts requires intentional recovery, while quieter periods offer opportunities to invest in relationships and personal growth.
The Current State of Nurse Burnout and Work-Life Challenges
Understanding the scope of current challenges helps contextualize why achieving balance remains difficult yet essential for the nursing profession.
Alarming Burnout Statistics
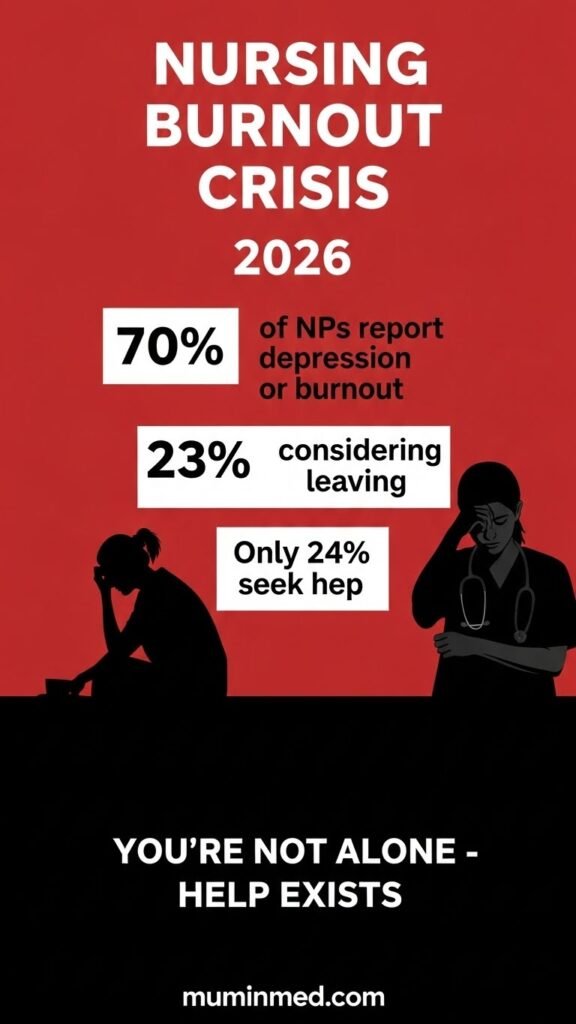
According to comprehensive 2024 workforce data, twenty-three percent of nurses are considering leaving the profession, according to Nurse.com, with registered nurses and licensed practical nurses showing the highest attrition risk. Survey data reveal that seventy percent of nurse practitioners report feeling depressed, burned out, or experiencing both conditions simultaneously, Statista.
The burnout crisis extends beyond individual Well-being:
In 2024, thirty-nine percent of nurses indicated their burnout had worsened compared to the previous year, despite increased awareness and conversation around mental health in nursing. Only twenty-four percent of nurses sought professional help for burnout or depression, with nearly forty percent never having done so, according to FRESHRN.
Primary Contributors to Nursing Stress
Research from 2024 identifies excessive bureaucratic tasks as the top burnout contributor, cited by sixty-two percent of nurse practitioners, according to FRESHRN. The constant documentation, policy compliance, and electronic health record management drain time and energy that nurses prefer dedicating to patient care.
Additional stressors include:
- Inadequate Staffing: Sixty-two percent of registered nurses reported increased workload during the pandemic, with forty-five percent feeling burned out, Oncology Nursing Society
- Poor Working Conditions: Fifty-five percent of nurse practitioners identify this as a major burnout factor
- Inadequate Compensation: Fifty-one percent cite insufficient pay relative to workload and responsibility
- Workplace Violence: Acute care nurses experience significantly higher rates of verbal abuse, intimidation, and physical assault
The Workforce Crisis Connection
Projections estimate that by 2026, the healthcare workforce will face a shortage of 200,000 to 450,000 nurses, according to the Oncology Nursing Society. Studies confirm that difficulty balancing work and home life increases nurses’ desire to leave their positions, according to PubMed Central, creating a self-perpetuating cycle where remaining staff face even greater burdens.
The Impact of Shift Work on Personal Life
Shift work represents one of the most significant challenges to maintaining balance in the nursing career. Understanding how different scheduling models affect Well-being helps nurses make informed choices about their work arrangements.
The 12-Hour Shift Model
Most hospital nurses work either 7 am to 7 pm or 7 pm to 7 am shifts, typically completing three twelve-hour shifts weekly for a total of thirty-six hours, according to the American Nurses Association.
Advantages of 12-Hour Shifts
More Days Off: Working three days weekly provides four consecutive days for recovery, family time, and personal pursuits. This extended break allows nurses to decompress from the emotional and physical demands of patient care.
Reduced Commuting: Fewer scheduled days mean less time and money spent traveling to work, according to the American Nurses Association, particularly beneficial for nurses living far from their healthcare facilities.
Enhanced Continuity of Care: Twelve-hour shifts reduce patient handoffs from three per day to two, improving information transfer and strengthening patient-nurse relationships.
Financial Incentives: Many facilities offer night shift differentials or weekend premiums, increasing earning potential for nurses willing to work less desirable hours.
Disadvantages of Extended Shifts
Studies demonstrate that nurses working shifts of ten hours or longer experience two and a half times greater likelihood of burnout and job dissatisfaction, according to Rasmussen University.
Physical Exhaustion: Twelve-hour shifts are associated with clear health risks, including Shift Work Sleep Disorder, which causes difficulty falling asleep, staying asleep, and can lead to cardiovascular complications, accidents, and unstable mood, according to Nursejournal.org.
Inadequate Self-Care: Long shifts make it challenging to maintain proper nutrition and hydration. Nurses often skip meals or rely on quick, unhealthy food options during demanding shifts.
Limited Personal Time: Extended shifts leave less time and energy for family and friends on work days, according to the American Nurses Association, potentially causing missed important family events and strained relationships.
Increased Error Risk: Research shows nurses working overtime or shifts longer than twelve hours experienced significantly more errors or near-errors, according to Rasmussen University.
The 8-Hour Shift Alternative
Eight-hour shifts remain standard in private practices and outpatient settings such as schools or physicians’ offices, according to Nursing CE Central.
Benefits of Shorter Shifts
Reduced Fatigue: Shorter workdays help nurses maintain alertness and decision-making capacity throughout their shifts, potentially reducing medication errors and patient safety incidents.
Better Daily Routine: Eight-hour shifts can result in decreased errors, less fatigue, and decreased rates of burnout, according to Nursing CE Central, by allowing nurses to maintain more regular sleep schedules and family routines.
Easier Self-Care: More reasonable shift lengths provide time for exercise, meal preparation, and adequate sleep between work days.
Drawbacks of Traditional Shifts
More Working Days: Eight-hour shifts typically require five days weekly, providing only traditional two-day weekends for personal time and recovery.
Increased Handoffs: More shift changes per day increase the risk of communication errors during patient handoffs, though proper protocols can mitigate this concern.
From my clinical experience, I’ve observed that shift preference varies significantly based on individual circumstances. Nurses with young children often prefer three consecutive long shifts to maximize consecutive days home, while those managing chronic health conditions may find shorter shifts more sustainable long-term.
[Comparison Table: Shift Types with specifications]
| Shift Type | Weekly Hours | Days Worked | Days Off | Best For | Main Challenge |
| 12-Hour | 36 hours | 3 days | 4 days | Maximizing consecutive time off; longer commutes | Physical exhaustion; limited daily personal time |
| 10-Hour | 40 hours | 4 days | 3 days | Balanced approach; moderate commutes | Still requires extended focus; fatigue risk |
| 8-Hour | 40 hours | 5 days | 2 days | Routine; outpatient settings | More commuting days; fewer extended breaks |
Evidence-Based Strategies for Achieving Balance
Maintaining a healthy balance during shift work requires intentional strategies supported by research and clinical best practices.
Strategy 1: Prioritize Sleep and Recovery
Establishing regular sleep and wake times, even on days off, helps maintain a consistent sleep schedule, according to NursingEducation critical for shift workers.
Practical Sleep Optimization:
- Create a sleep-conducive environment by controlling light exposure, minimizing noise, and maintaining comfortable temperatures
- Consider short fifteen to thirty-minute power naps before shifts to help energize you
- Limit caffeine intake at least six hours before intended sleep time
- Use blackout curtains and white noise machines for daytime sleep after night shifts
- Avoid alcohol, which disrupts sleep quality despite seeming to help with initial drowsiness
From my years working night shifts in the ICU, I learned that consistent sleep schedules—even on days off—dramatically improved my energy levels and cognitive function during subsequent shifts.
Strategy 2: Establish Clear Boundaries
Setting boundaries involves creating clear schedules for when you work and when you don’t, both literally and figuratively.
Boundary-Setting Practices:
- Avoid checking work emails or messages during off-duty hours unless you’re on-call
- Learn to say no to additional shifts when you need recovery time, according to WGU, recognizing that declining requests isn’t selfish but necessary for sustained performance.
- Create transition rituals that help mentally separate work from home, such as changing clothes immediately upon arriving home or taking a short walk.
- Communicate your availability clearly with both colleagues and family members.
- Resist the temptation to pick up extra shifts during periods when recovery is essential.
Strategy 3: Implement Effective Time Management
Effective time management allows nurses to allocate dedicated periods for self-care activities, including exercise, relaxation, hobbies, and spending time with loved ones.
Time Management Techniques:
- Batch Similar Tasks: Group similar activities like meal preparation, errands, or administrative tasks to maximize efficiency
- Use Planning Tools: Digital calendars or planning apps help visualize commitments and identify available personal time
- Schedule Self-Care: Treat exercise, hobbies, and relaxation as non-negotiable appointments rather than optional activities
- Prepare in Advance: Pack meals and work bags the night before to reduce morning stress.
- Protect Transition Time: Build buffer periods between work and personal activities for mental transitions.
Strategy 4: Optimize Nutrition and Hydration
Nursing requires substantial energy and a supported immune system to protect against daily stressors, achieved through adhering to a nourishing diet, according to Alliant University.
Nutritional Strategies for Shift Workers:
- Batch cooking or meal prepping saves time during the work week by preparing nutritious meals for lunch and dinner in advance
- Pack protein-rich snacks like nuts, cheese, hard-boiled eggs, or protein bars for sustained energy during shifts
- Studies show diets high in antioxidant-rich vegetables and omega-3 fats may help moderate cortisol levels, reducing stress impact.
- Keep a reusable water bottle accessible during shifts, setting hourly hydration reminders if necessary.
- Plan post-shift meals to avoid unhealthy convenience foods when exhausted.
During my emergency department years, I found that preparing mason jar salads and grain bowls on my days off ensured I had nutritious options even during the most demanding weeks.
Physical Health and Wellness Practices
Physical Well-being forms the foundation for sustainable nursing practice and personal life satisfaction.
Exercise and Movement
Regular exercise relieves stress and increases energy levels, with activities like walking, jogging, swimming, yoga, or weight lifting lowering disease risk.
Exercise Strategies for Busy Nurses:
- Micro-Workouts: Ten to fifteen-minute activity sessions fit more easily into demanding schedules than hour-long gym sessions
- Active Commuting: Walking or cycling to work when feasible combines transportation with physical activity
- Stretching Between Patients: Brief stretching during shift transitions reduces musculoskeletal strain
- Home Workouts: YouTube fitness channels and fitness apps eliminate commute time to gyms
- Activity Tracking: Pedometers or fitness trackers provide motivation and accountability
Recommended Weekly Activity Levels: According to CDC guidelines, adults should aim for 150 minutes of moderate-intensity aerobic activity plus two days of muscle-strengthening activities weekly. For nurses, breaking this into manageable segments—such as three ten-minute walks daily—makes goals more achievable.
Musculoskeletal Health
Nursing’s physical demands—lifting patients, prolonged standing, awkward positions—create significant injury risk. Protecting your body requires:
- Proper Body Mechanics: Always use lift equipment and request assistance for patient transfers
- Supportive Footwear: Invest in high-quality nursing shoes with adequate arch support and cushioning
- Core Strengthening: Regular core exercises prevent back injuries common in nursing
- Stretching Routines: Daily stretching, particularly for the neck, shoulders, and lower back, prevents cumulative strain
- Ergonomic Awareness: Adjust computer stations and documentation areas to reduce repetitive strain
Preventive Healthcare
Taking time off work for regular self-check-ins and remaining current on vaccinations ensures you can continue caring for patients and meeting personal life demands.
Essential Preventive Measures:
- Schedule annual physical examinations and recommended screenings
- Maintain current vaccinations, including annual influenza vaccines
- Address minor health concerns promptly before they escalate
- Utilize employee health services for occupational health monitoring
- Practice good hand hygiene and infection control to protect personal health
Mental and Emotional Well-being
The emotional demands of nursing—witnessing suffering, making life-affecting decisions, managing difficult family dynamics—require dedicated mental health practices.
Recognizing Compassion Fatigue and Burnout
Burnout results from unmanaged stress and can manifest as exhaustion, lack of motivation, and negative feelings toward your job.
Warning Signs to Monitor:
- Persistent physical and emotional exhaustion even after days off
- Cynicism or detachment from patients and colleagues
- Reduced sense of professional accomplishment
- Increased irritability with patients, families, or coworkers
- Physical symptoms like headaches, gastrointestinal issues, or frequent illnesses
- Difficulty concentrating or making decisions
- Withdrawal from social connections
- Using unhealthy coping mechanisms like excessive alcohol consumption
Stress Management Techniques
Behavioral strategies include goal setting, problem-solving, and behavioral activation through increasing enjoyable, valued, and goal-oriented activities, according to PubMed Central.
Evidence-Based Stress Reduction:
Mindfulness and Meditation: Research demonstrates that mindfulness meditation can reduce stress and feelings of burnout while increasing resiliency, according to the Oncology Nursing Society. Simple practices include:
- Five-minute breathing exercises before or after shifts
- Guided meditation apps like Headspace, Calm, or Insight Timer
- Mindful walking during breaks, focusing on physical sensations
- Body scan meditations before sleep
Cognitive Behavioral Techniques: Cognitive behavioral interventions help nurses address work-related stressors and improve work-life balance by protecting time with family and friends PubMed Central. This includes:
- Identifying and challenging negative thought patterns
- Reframing difficult situations to find meaning and growth opportunities
- Setting realistic expectations for yourself and others
- Practicing self-compassion rather than self-criticism
Professional Mental Health Support: Nearly forty percent of nurses have never sought professional help for burnout or depression, despite its effectiveness. Seeking support from licensed therapists, particularly those specializing in healthcare worker wellness, provides valuable tools for managing occupational stress.
Emotional Processing
Decompression Rituals: Creating relaxing routines before and after shifts helps decompress from work stress. Examples include:
- Journaling about difficult shifts to process emotions
- Listening to calming music during commutes
- Taking warm baths or showers to mark transitions between work and home
- Engaging in creative outlets like art, music, or writing
Peer Support: Discussing challenging cases with trusted colleagues who understand nursing’s unique stressors provides validation and perspective. Many hospitals offer peer support programs specifically for processing difficult patient outcomes.
Time Management and Boundary Setting
Nursing career balance strategies depend heavily on how effectively you manage limited time and protect personal boundaries.
Advanced Time Management Principles
The Eisenhower principle distinguishes between urgent and important tasks, recognizing that urgent matters aren’t always important, while important priorities rarely feel urgent.
Priority Matrix Application for Nurses:
Important and Urgent: Patient emergencies, critical family needs, acute health issues
- Action: Address immediately with full attention
Important but Not Urgent: Exercise, continuing education, relationship building, preventive healthcare
- Action: Schedule specific times and protect these commitments
Urgent but Not Important: Many emails, some meetings, minor requests
- Action: Delegate when possible or handle efficiently without extended time investment
Neither Important nor Urgent: Excessive social media, unnecessary meetings, time-wasting activities
- Action: Minimize or eliminate to create space for meaningful activities
Boundary Protection Strategies
Many people, especially those with generous, caring hearts, find telling someone no extremely difficult, worrying that declining is selfish or will disappoint others, according to WGU. However, occasional refusals prove essential for prioritizing Well-being and managing time efficiently.
Effective Boundary-Setting Language:
- “I appreciate you thinking of me, but I’m not available that day.”
- “I need to check my schedule and get back to you.”
- “I’m focusing on family time this weekend.”
- “I’ve committed to self-care activities during my days off.”
- “I’m not able to take on additional shifts right now.”
Digital Boundaries:
- Disable work-related notifications during off hours.
- Use separate devices or profiles for work and personal communications
- Set email auto-responses indicating your availability
- Resist checking work messages during personal time unless you’re on-call
Saying No Without Guilt
Occasionally, saying no is essential to prioritizing your well-being and managing your time efficiently. Remember:
- Declining extra shifts protects your ability to provide quality care during scheduled shifts
- Your health and family deserve protection just as much as your patients need care
- Sustainable careers require periods of rest and recovery
- Saying yes to everything leads to burnout, ultimately reducing your availability long-term
Building Support Systems
Building a support network of colleagues, friends, and family helps nurses manage stress and maintain work-life balance, according to the NSHCOA.
Professional Support Networks
Colleague Connections: Fellow nurses understand the unique challenges of healthcare work. Cultivating supportive workplace relationships provides:
- Emotional validation during difficult shifts
- Practical advice for managing specific unit challenges
- Shift coverage during personal emergencies
- Professional growth through shared learning
Mentorship Relationships: Nurse mentors or friends in healthcare can offer advice to help you through challenging times or lighten your workload. Both being mentored and mentoring others enrich professional life.
Professional Organizations: Membership in specialty nursing associations provides:
- Continuing education opportunities
- Networking with nurses facing similar challenges
- Resources for career advancement
- Advocacy for improved working conditions
Personal Support Systems
Family and Friends: Taking time to reconnect with family and friends is vital to maintaining a healthy work-life balance. Strategies include:
- Scheduling regular phone calls or video chats with distant loved ones
- Planning activities together during days off
- Communicating your work schedule clearly so others understand your availability
- Involving family in self-care activities when possible
Community Connections: Activities outside healthcare provide perspective and fulfillment:
- Religious or spiritual communities
- Hobby groups or classes
- Volunteer opportunities unrelated to nursing
- Neighborhood connections and local activities
Support for Family Caregivers
Fifty percent of nurses revealed they felt more pressured due to family responsibilities, and that career development slowed because of these obligations. Seventy percent felt it was difficult to manage household and office work when they had small kids.
Balancing Family Caregiving:
- Most nurses favored flexible work arrangements to manage household and office responsibilities and expected organizations to provide childcare facilities and flexible working hours
- Investigate employer childcare benefits or subsidies
- Build reciprocal childcare arrangements with other nursing families
- Communicate clearly with family about your energy levels after shifts
- Lower housekeeping standards during particularly demanding work periods
Organizational Strategies for Healthcare Institutions
While individual strategies are essential, healthcare organizations have a vital function in fostering nurses’ work-life balance through implementing flexible scheduling, ensuring adequate staffing, and fostering positive work environments, according to the NSHCOA.
Evidence-Based Institutional Interventions
Flexible Scheduling Options:
- Self-scheduling systems that allow nurses greater control over work patterns
- Shift swapping platforms facilitating peer-to-peer schedule trades
- Part-time and per diem positions for nurses needing reduced hours
- Compressed workweeks offering alternative scheduling models
- Gradual return-to-work programs following leaves of absence
Adequate Staffing Levels: Proper nurse-to-patient ratios represent perhaps the most critical factor affecting work-life balance. High turnover contributes to increased burnout among remaining faculty, furthering the supply-demand gap in the nursing workforce, according to the Oncology Nursing Society.
California’s mandated nurse-patient ratios demonstrate that regulatory requirements can improve working conditions, though nationwide adoption remains controversial.
Workplace Wellness Programs:
- Employee assistance programs provide confidential counseling
- Stress management workshops and resilience training
- Mindfulness programs and meditation spaces
- Physical wellness initiatives, including gym memberships or on-site fitness facilities
- Mental health days are separate from sick leave
Supportive Leadership: Fifty-two percent of nurses felt unsupported at work in 2023, according to Nurse.org, indicating significant room for improvement in management practices.
Effective nurse leadership includes:
- Regular check-ins addressing workload concerns
- Recognition programs celebrating nursing contributions
- Transparent communication about organizational decisions
- Input opportunities for bedside nurses in policy development
- Zero-tolerance policies for workplace violence and harassment
Reducing Administrative Burden
Sixty-two percent of nurse practitioners cited excessive bureaucratic tasks as their top burnout contributor. Healthcare organizations can:
- Streamline documentation requirements
- Improve electronic health record usability
- Employ unit secretaries to handle non-clinical administrative tasks
- Implement voice-to-text documentation systems
- Regularly evaluate which documentation adds value versus compliance burden
Creating Your Personal Balance Plan
Achieving a realistic work-life balance in the nursing profession requires personalized strategies reflecting your unique circumstances, values, and priorities.
Self-Assessment Exercise
Begin by honestly evaluating your current situation:
Current State Analysis:
- How many hours do you work weekly (including overtime)?
- How many days typically pass between your last work shift and feeling fully rested?
- When did you last engage in a hobby or leisure activity you enjoy?
- How would you rate your physical health on a scale of 1-10?
- How would you describe your stress levels?
- Are your important relationships thriving, struggling, or somewhere between?
- What activities bring you joy that you’re currently not doing?
Values Clarification: Identify your top five values (examples: family time, professional excellence, physical health, financial security, creative expression, community involvement, spiritual growth). Your balance plan should align with these priorities.
Developing Your Action Plan
Step 1: Set Specific Goals Rather than vague intentions like “exercise more,” create measurable objectives:
- “Walk 20 minutes three times weekly.”
- “Prepare healthy lunches every Sunday for the work week.”
- “Schedule monthly date nights with my partner.r”
- “Complete 15 minutes of meditation four times weekly.”
Step 2: Identify Required Resources. What do you need to achieve your goals?
- Time (which activities can you reduce or eliminate?)
- Money (what’s your budget for wellness investments?)
- Support (who can help you succeed?)
- Information (what knowledge or skills do you need?)
- Physical resources (equipment, space, tools)
Step 3: Anticipate Obstacles. Common barriers for nurses include:
- Unpredictable scheduling
- Physical exhaustion after shifts
- Guilt about prioritizing personal needs
- Financial constraints
- Lack of accessible support
For each obstacle, develop contingency plans:
- “If my shift runs late, I’ll do a 10-minute workout instead of 30 minutes.”
- “If I’m too tired to cook, I’ll have healthy frozen meals as backup.”
- “If childcare falls through, I’ll do a family activity instead of solo exercise.”
Step 4: Track Progress and Adjust. Evaluating and adapting your schedule as needed is an important part of building a plan that works for you.
- Use a simple tracking method (app, journal, or calendar)
- Review weekly: What worked? What didn’t? What needs adjustment?
- Celebrate small wins to maintain motivation
- Be flexible—perfection isn’t the goal; sustainable improvement is
Sample Weekly Balance Plan
For a Nurse Working Three 12-Hour Shifts (Monday, Tuesday, Wednesday):
Monday-Wednesday (Work Days):
- Wake 2 hours before shift for breakfast and mental preparation
- Pack nutritious meals and snacks
- Take all scheduled breaks, using 15 minutes for brief walks or stretching
- Transition ritual: 10-minute meditation or music listening after clocking out
- Simple dinner, hydration, gentle stretching
- Sleep 8 hours minimum
Thursday (Recovery Day):
- Sleep in if needed
- Light activity only (gentle yoga, short walk)
- Meal prep for the upcoming week
- Catch up on personal tasks
- Early bedtime to restore sleep debt
Friday-Sunday (Active Days Off):
- Friday: Exercise 30-45 minutes, social activity or hobby
- Saturday: Family time, community involvement, or personal interests
- Sunday: Meal prep, planning for the week ahead, relaxation
Daily Non-Negotiables (All Days):
- 8 hours of sleep opportunity
- Three balanced meals
- Hydration (aim for 8 glasses of water)
- 10 minutes of outdoor time
- Connection with at least one supportive person
This framework adjusts based on your specific schedule, family obligations, and preferences.
Frequently Asked Questions
Q: How do nurses working 12-hour shifts maintain work-life balance when they’re exhausted on work days?
A: The flexibility of working three days followed by four days off may offer nurses better work-life balance, allowing time for personal needs such as attending doctors’ appointments, home maintenance, banking, and caring for family members, according to the American Nurses Association. The key is accepting that work days focus primarily on job performance and basic self-care, while days off provide opportunities for enrichment activities. Prioritize sleep, simple meals, and brief decompression rituals on work days, saving energy-intensive activities for your extended time off.
Q: What’s the best shift schedule for maintaining family life—8-hour or 12-hour shifts?
A: No universal answer exists; the optimal schedule depends on your family structure and priorities. Many nurses prefer to schedule “weekends” between their 12-hour shifts, working Monday, Tuesday, and Friday while taking off the two-day periods in between, according to the American Nurses Association. Nurses with school-age children often prefer extended consecutive days off to participate in activities and trips, while those with infants might find shorter daily shifts easier for maintaining feeding schedules and shared parenting responsibilities. Evaluate what works for your specific situation.
Q: How can night shift nurses achieve adequate sleep?
A: Shift Work Sleep Disorder impacts a considerable number of workers with nontraditional schedules and can result in difficulty falling asleep, staying asleep, or sleeping when individuals want or need to, according to Nursejournal.org. Strategies include maintaining consistent sleep-wake times even on days off, using blackout curtains and white noise machines, keeping bedroom temperature cool, avoiding screens before sleep, and educating family members about respecting your sleep schedule. Consider short naps before shifts to boost alertness.
Q: What should I do if I’m experiencing burnout?
A: Recognize that burnout results from unmanaged stress and can manifest as exhaustion, lack of motivation, and negative feelings toward your job. First, talk with your supervisor about workload concerns and available resources like employee assistance programs. Only twenty-four percent of nurses sought professional help for burnout or depression, according to FRESHRN, yet therapy provides valuable coping strategies. Consider whether schedule changes, time off, or role adjustments might help. Remember that addressing burnout isn’t weakness—it’s professional self-care that ultimately benefits your patients.
Q: How can I say no to picking up extra shifts without feeling guilty?
A:
Occasionally, saying no is essential to prioritizing your well-being and managing your time efficiently, and it’s important to recognize that you can’t be everything to everyone. Frame declining as protecting your ability to provide quality care during scheduled shifts. You might say, “I appreciate you thinking of me, but I have commitments during my time off that I need to honor.” Remember that consistently picking up shifts when you need rest leads to burnout, ultimately making you less available long-term.
Q: What are effective ways to decompress after particularly difficult shifts?
A: Creating relaxing routines before and after shifts can help you decompress from work stress, whether this involves taking a warm bath, practicing deep breathing, or engaging in a hobby you enjoy. Develop personalized transition rituals such as listening to specific music during your commute, changing immediately into comfortable clothes, or taking a brief walk outside. For especially traumatic shifts, talk with colleagues who understand, journal your feelings, or contact employee assistance programs for additional support. Avoid immediately discussing difficult cases with family members who may not have the context to understand.
Q: How can I maintain physical fitness with an unpredictable nursing schedule?
A: Effective time management is the key to work-life balance and managing stress, allowing you to allocate dedicated time for self-care activities like exercise. Focus on consistency over intensity—three 15-minute workouts weekly provide more benefit than sporadic hour-long sessions. Choose activities requiring minimal setup, like bodyweight exercises, walking, or online workout videos. Schedule exercise as non-negotiable appointments. On exhausting work days, gentle movement like stretching counts as success. Build activity into daily routines through parking farther away, taking stairs, or walking during breaks.
Q: Should I pursue additional certifications if I’m struggling with work-life balance?
A: Additional credentials can enhance career satisfaction and potentially lead to roles with better schedules or autonomy. However, pursuing certifications while experiencing burnout may worsen stress. First, establish baseline balance through the strategies outlined in this article. Once you feel stable, certifications in areas like nurse practitioner, clinical nurse specialist, or specialty certifications (critical care, oncology, etc.) might open doors to positions better aligned with your work-life priorities. Evaluate whether the temporary increased stress of education will lead to long-term improvements in your balance.
Q: How do I handle family members who don’t understand my need for recovery time after shifts?
A: Education is key. Explain that 12-hour shifts involve constant decision-making, physical exertion, and emotional labor equivalent to running a mental and physical marathon. Share specific examples: “I walked 8 miles during my shift while monitoring critically ill patients, managing emergencies, and supporting grieving families—I need time to recover before I can be fully present with you.” Taking time to reconnect with family and friends is vital to maintaining a healthy work-life balance, but good relationships have boundaries. Set clear expectations about your energy levels on work days versus days off, and involve family in creating sustainable routines.
Q: What are the signs that my workplace is contributing to poor work-life balance beyond what I can control?
A: Red flags include persistently unsafe staffing ratios, mandatory overtime exceeding occasional emergencies, management dismissing concerns about workload, lack of meal or rest breaks, workplace violence without organizational response, or punitive reactions to time-off requests. Fifty-two percent of nurses felt unsupported at work, according to Nurse.org. If your workplace consistently fails to provide reasonable working conditions despite your boundary-setting efforts, it may be time to explore other employment options. Your long-term health and career sustainability matter more than loyalty to an organization that doesn’t support staff Well-being.
Q: How can new graduate nurses establish work-life balance from the start of their careers?
A: New nurses should prioritize learning effective time management, boundary-setting, and self-care habits early before burnout develops. Focus on one unit for your first year to develop competence and routine. Resist pressure to work excessive overtime while still developing skills. Find a mentor who models healthy balance. Remember that slower initial skill development is normal—don’t sacrifice your Well-being trying to perform at experienced nurse levels immediately. Build recovery time into your schedule and protect days off for genuine rest rather than filling them with activities. The habits you establish now set patterns for your entire career.
Q: Are there specific medical devices or apps that can help nurses maintain work-life balance?
A: Several technologies support nursing wellness:
Fitness Trackers (Fitbit, Apple Watch, Garmin): Monitor activity, sleep quality, and stress levels while providing reminder alerts for movement and hydration.
Meditation Apps (Headspace, Calm, Insight Timer): Offer guided meditations, breathing exercises, and sleep stories specifically designed for healthcare workers.
Meal Planning Apps (Mealime, Prepear, Plan to Eat): Streamline nutrition by organizing recipes, generating shopping lists, and suggesting quick, healthy meals.
Sleep Optimization Tools: White noise machines, smart alarm clocks (like Phillips SmartSleep), and sleep tracking apps help maximize rest quality despite irregular schedules.
Scheduling Apps (Google Calendar, Shift work Calendar): Help visualize work patterns and plan personal activities around demanding schedules.
While no device replaces fundamental self-care practices, these tools provide structure and accountability that many nurses find helpful.
Conclusion
Achieving work-life balance as a registered nurse represents one of healthcare’s most persistent challenges, yet it remains essential for both personal well-being and professional longevity. As someone who has navigated emergency rooms, intensive care units, pediatric wards, and general medical floors over the past decade, I can attest that balance isn’t a destination but an ongoing practice requiring intention, flexibility, and self-compassion.
Recent studies confirm that the struggle is real, with over twenty percent of nurses working 41-50 hours weekly and many experiencing significant burnout, according to the Oncology Nursing Society. Yet research and clinical experience also demonstrate that a realistic work-life balance in the nursing profession is achievable through evidence-based strategies.
The foundations of a balanced lifestyle for full-time nurses include:
- Prioritizing adequate sleep and physical recovery
- Setting and maintaining firm boundaries
- Implementing effective time management
- Building robust support networks
- Advocating for organizational improvements
- Customizing strategies to your unique circumstances
Remember that maintaining a healthy balance during shift work isn’t selfish—it’s essential healthcare. Healthcare organizations have a vital function in fostering nurses’ work-life balance, but you must also take personal responsibility for protecting your well-being.
Whether you’re just beginning your nursing journey or reassessing priorities mid-career, start with small, sustainable changes. You don’t need to implement every strategy simultaneously. Choose two or three that resonate most strongly, establish them as habits, then gradually add others.
Your patients need you at your best, and you deserve a fulfilling life beyond nursing. Work-life harmony for healthcare professionals isn’t about perfection but about creating sustainable patterns that honor both your calling to care for others and your right to care for yourself.
Medical Disclaimer: This article is for informational purposes only and does not constitute medical advice. Abdul-Muumin Wedraogo is a Registered General Nurse, but recommendations should not replace consultation with your healthcare provider. Always consult with a qualified physician or healthcare professional before starting any new supplement, diet, or treatment regimen, especially if you have existing medical conditions or take medications.
Acknowledgments
I would like to thank my colleagues in emergency, intensive care, pediatric, and general ward nursing across Ghana Health Service facilities for their valuable insights during the preparation of this article. Your shared experiences of balancing demanding clinical responsibilities with personal lives have informed these recommendations. I also acknowledge the medical research community for their continued work in studying nurse Well-being and work-life balance, and the professional organizations—particularly the Nurses and Midwifery Council, Ghana, and the Ghana Registered Nurses and Midwives Association—that advocate for improved working conditions. Finally, thank you to the readers seeking to create more sustainable, fulfilling nursing careers.
References
- American Nurses Association. (2024). Nursing workforce statistics 2024. Retrieved from https://www.nursingworld.org
- Adriaenssens, J., De Gucht, V., & Maes, S. (2015). Determinants and prevalence of burnout in emergency nurses: A systematic review of 25 years of research. International Journal of Nursing Studies, 52(2), 649-661. https://doi.org/10.1016/j.ijnurstu.2014.11.004
- Trybou, J., Gemmel, P., & Annemans, L. (2014). The ties that bind: An integrative framework of physician-hospital alignment. BMC Health Services Research, 14, 1-17. https://doi.org/10.1186/1472-6963-14-1
- Dall’Ora, C., Ball, J., Reinius, M., & Griffiths, P. (2020). Burnout in nursing: A theoretical review. Human Resources for Health, 18(1), 1-17. https://doi.org/10.1186/s12960-020-00469-9
- Labrague, L. J., Al Sabei, S. D., AbuAlRub, R., Burney, I. A., & Al Rawajfah, O. (2021). Work-life balance among nurses: a literature review. Indian Journal of Continuing Nursing Education, 22(1), 65-71.
- Agency for Healthcare Research and Quality. (2024). Combating burnout in nursing. US Department of Health and Human Services. Retrieved from https://www.ahrq.gov
- Centers for Disease Control and Prevention. (2024). How much physical activity do adults need? Retrieved from https://www.cdc.gov/physicalactivity
- Maslach, C., & Leiter, M. P. (2016). Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry, 15(2), 103-111. https://doi.org/10.1002/wps.20311
- World Health Organization. (2024). Burnout is an “occupational phenomenon”: International Classification of Diseases. Retrieved from https://www.who.int
- National Institute for Occupational Safety and Health. (2024). Work schedules: Shift work and long hours. Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/niosh
- Rogers, A. E., Hwang, W. T., Scott, L. D., Aiken, L. H., & Dinges, D. F. (2004). The working hours of hospital staff nurses and patient safety. Health Affairs, 23(4), 202-212. https://doi.org/10.1377/hlthaff.23.4.202
- Press Ganey Associates. (2024). 2024 nursing special report: The state of nursing. Retrieved from https://www.pressganey.com
- McHugh, M. D., Aiken, L. H., Sloane, D. M., Windsor, C., Douglas, C., & Yates, P. (2021). Effects of nurse-to-patient ratio legislation on nurse staffing and patient mortality, readmissions, and length of stay: A prospective study in a panel of hospitals. The Lancet, 397(10288), 1905-1913. https://doi.org/10.1016/S0140-6736(21)00768-6
- American Association of Nurse Practitioners. (2024). 2024 National Nurse Practitioner Survey Results. Retrieved from https://www.aanp.org
About the Author
Abdul-Muumin Wedraogo, RGN, BSN, is a Registered General Nurse with over 10 years of clinical experience across Emergency, Pediatric, Intensive Care, and General Ward settings with the Ghana Health Service. He holds a Bachelor of Science in Nursing from Valley View University and graduated from Premier Nurses’ Training College, Ghana. Abdul-Muumin is a certified member of the Nurses and Midwifery Council (NMC), Ghana, and the Ghana Registered Nurses and Midwives Association (GRNMA).
Throughout his decade in healthcare, Abdul-Muumin has witnessed firsthand the challenges nurses face in maintaining work-life balance while providing exceptional patient care. His experience spanning high-intensity emergency departments to long-term care settings has given him unique insights into the strategies that work across different nursing specialties and practice environments.
Beyond his clinical work, Abdul-Muumin combines his healthcare expertise with technology insights (Diploma in Network Engineering, Advanced Professional in System Engineering) to provide evidence-based reviews of medical devices and health products at Muminmed.com. His mission is to help healthcare professionals make informed decisions about tools and strategies that support both patient care excellence and personal well-being.








